Managing Insurance Claims
![]() Related Training
Related Training
Managing Insurance Claims Recorded Class
Pre-Authorizations Recorded Class
Submitting Secondary Insurance Claims Recorded Class
To manage claims for a location or for all locations in a practice, use the Claims Management window. From the Location tab, select Claims > Claims Management. The Claims Management window is displayed, listing the claims for the location.
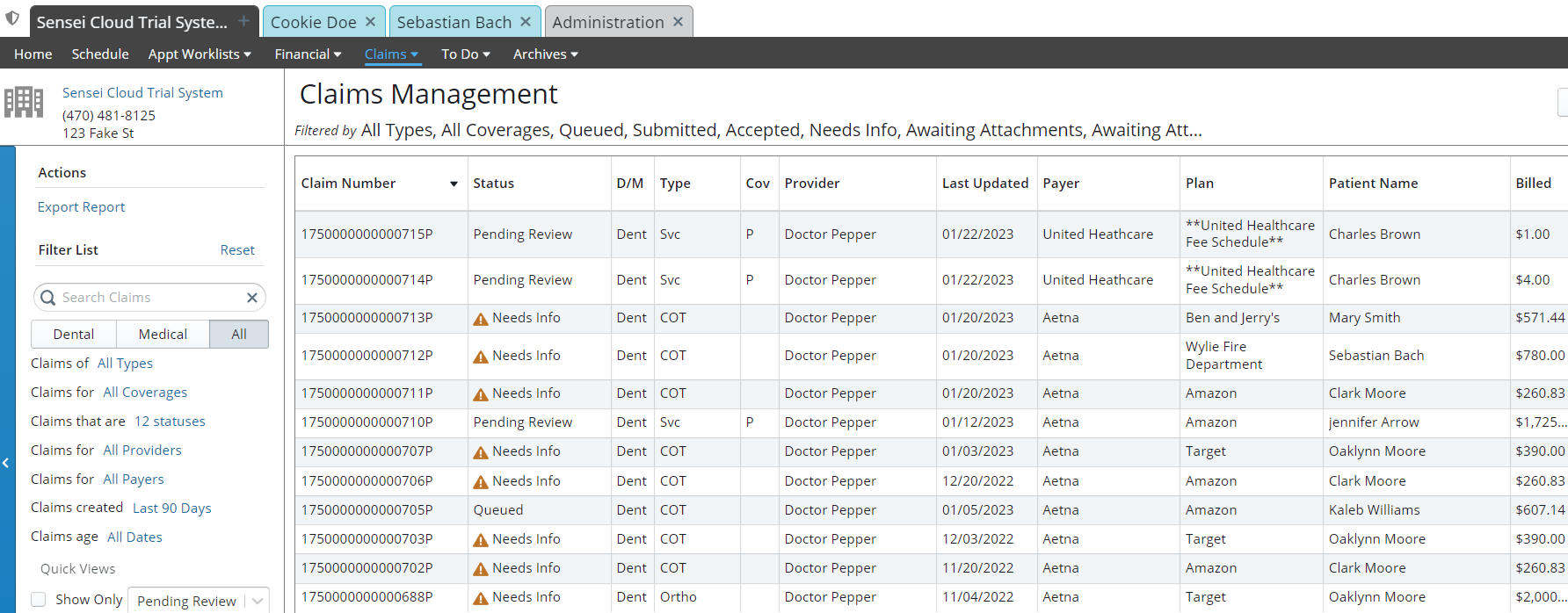
For each claim, you can view the Claim Number, Status, D/M (dental/medical), Claim Type, COV (primary or secondary), Provider, Last Updated Date, Payer, Plan, Patient Name, Billed Amount, and Paid Amount.
You can:
-
Sort the list by any column.
-
Search claims by patient, policyholder, claim ID, and procedure code.
-
Display only the claims that are cancelled, pending review, or awaiting attachments.
-
Click the Export Report option to create a .CSV file of the list.
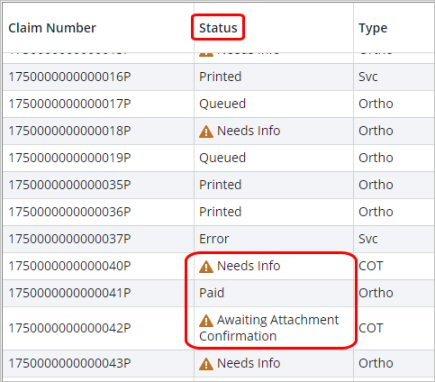
Claims that require action display an Alert icon in the Status column.
The claim type is assigned automatically when a claim is generated:
-
Svc—Statement of actual services
-
Pre-Auth—Request for pre-authorization
-
COT—Continuation of treatment for orthodontic services
-
Ortho—Initial claim for orthodontic treatment
To view a claim summary, select a claim in the list. The Claim Summary window is displayed.
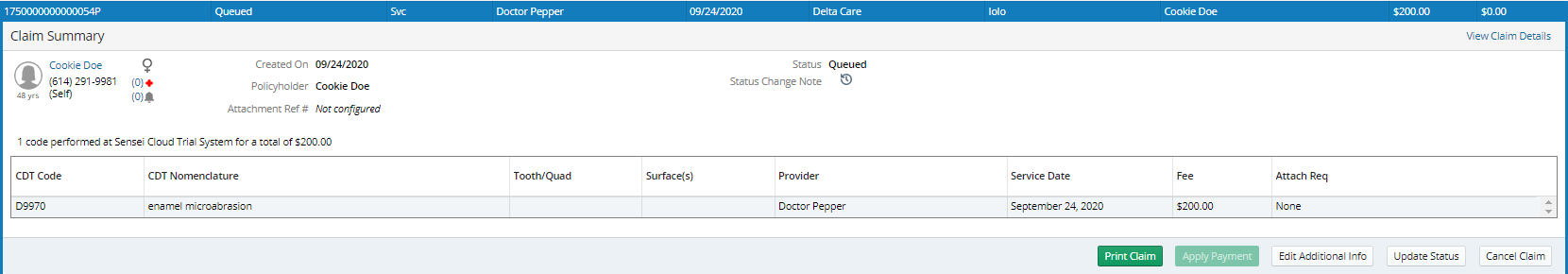
In the Claim Summary window, you can:
-
View the claim details
-
Enter a pre-authorization reference number
-
Submit unsubmitted claims
-
Print claims
-
Apply payments
-
Edit additional information
-
Update the claim status
- Cancel the claim
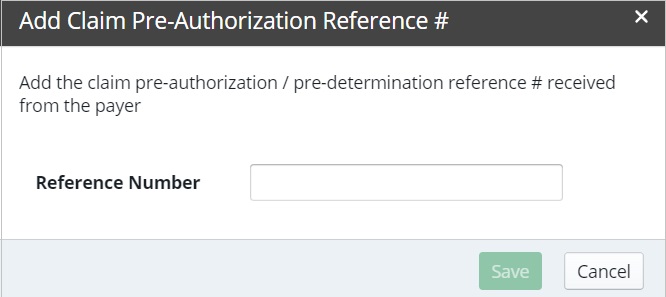
Adding a Pre-Authorization Reference Number
You can manually add a pre-authorization number that was received from an insurance payer from a portal, phone call, fax, and so on, to both medical and dental insurance claims.
To add a pre-authorization number to a claim:
-
On the Patient tab, select Insurance > Claims Management.
-
Select the appropriate claim. The Claim Summary is displayed.
-
Click Add Reference #. The Add Claim Pre-Authorization Reference # window is displayed.
-
Type the reference number, and click Save. The saved pre-authorization number is automatically populated on dental and medical claims, paper and electronic.
Note: If you need to edit the pre-authorization reference number, click the number in the Claim Summary to display the Add Claim Pre-Authorization Reference # window and make the changes.
Setting Coverage Details and Benefits by Category on an Insurance Plan
Importing Coverage Details to an Insurance Plan
Setting Up Insurance Claim Processing
Canceling and Resubmitting Insurance Claims
Using ICD-10 Medical Diagnosis Codes and Submitting Medical Claims
Using CPT Codes for Medical Billing
Viewing Insurance Claims Statistics