Working with Insurance Carriers > Working with Insurance Plans
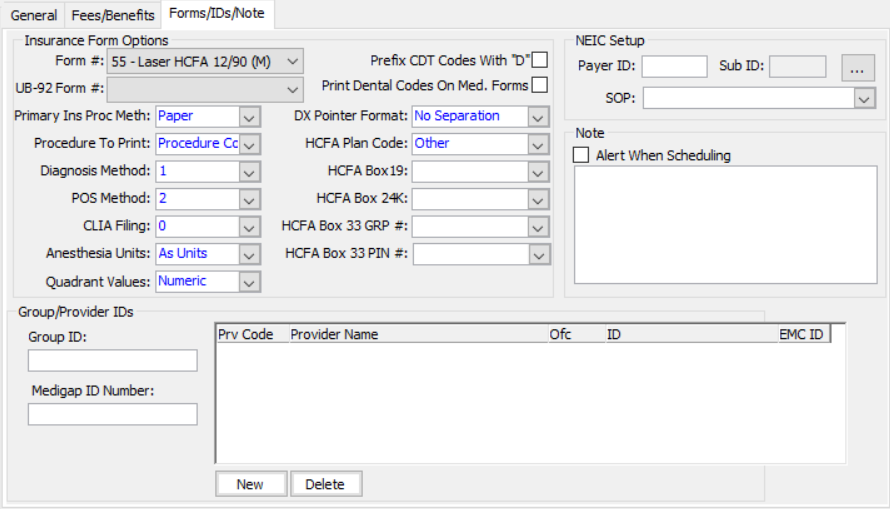
Use the Forms/IDs/Note tab of the Plan Data Entry window to provide information about insurance forms, group and provider IDs, and electronic claims setup.
To add a form, ID, or note:
Select Tables > Insurance > Plans. A list of plans is displayed.
Enter search criteria to find and select the plan.
Click the Forms/IDs/Note tab.
In the Insurance Form Options section, set these options:
Form #—Applies an insurance format based on whether the coverage is medical or dental.
UB-92 Form #—Applies an applicable UB-92 format. If the plan does not accept UB-92 billing, leave this field blank.
Primary Ins Proc Method—Select whether claims will be processed by Paper or Electronic.
Procedure to Print—Sets a coding method.
Diagnosis Method—Sets the method to print reference numbers or codes:
1—Prints reference numbers.
2—Prints ICD codes in HCFA box 24E.
3—Does not print ICD codes.
POS Method—Sets the method to print place-of-service codes:
1—Prints single-digit place-of-service codes.
2—Prints double-digit place-of-service codes.
In the CLIA Filing field, the default is 0. Select Provider, Office, or Practice.
In the Anesthesia Units field, set to As Units or To Minutes, based on the plan's billing requirements for drugs used for anesthesia.
For ADA paper forms 110 and 111, the Quadrant Values field is active. The default is Numeric. Change this to Alpha for insurance plans that require alpha characters for quadrant values.
Select the Prefix CDT Codes with “D” option to have the software replace the leading zero of your dental codes with a D on insurance claims for this plan.
Note: Dental codes posted using leading zeros instead of a D continue to display the leading zero in the ledger.
Select the Print Dental Codes on Med. Forms option to include dental procedures on medical claim forms for this plan.
Select the print options for medical forms from these drop-down lists:
HCFA Plan Code
HCFA Box 19
HCFA Box 24K
CMS 1500 (08/05) 33a
CMS 1500 (08/05) 33b
If you use the WinOMS electronic claim processing service, complete the fields in the NEIC Setup section:
In the Payor ID field, type a payor identification number.
In the Sub ID field, type a payor sub-identification number provided by NEIC.
From the SOP drop-down list, select a payment method.
To display a note automatically when scheduling a patient who has a policy that uses this insurance plan, select Alert When Scheduling, and type a note in the space provided.
In the Group ID and Medigap ID Number fields, type the ID numbers.
If you need to enter individual provider IDs, click New. The New Provider/Office/Plan ID window is displayed.
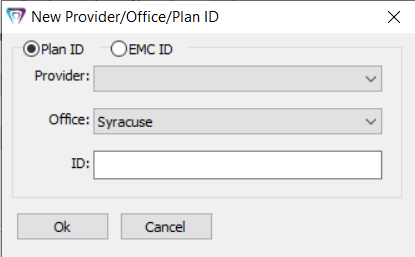
Select the Plan ID or EMC ID option. Use EMC ID only for carriers that require it. This option requires the EMC provider ID to appear in BAO, YAO, and BA1.
Set these options:
Provider—Name of the individual provider of services
Office—Office where services are provided
ID—Identification number
Click Ok.
Adding Fee and Benefit Information
Working with Fee and Allowable Schedules
Setting Up Insurance Estimating