Code-specific insurance plans offer coverage based on specific dental codes. The coverage may be either a specific amount or a percentage of UCR fees.
To set up an employer/plan that offers code-specific coverage:
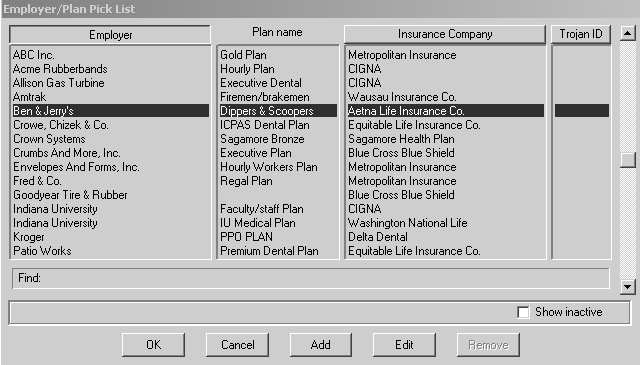
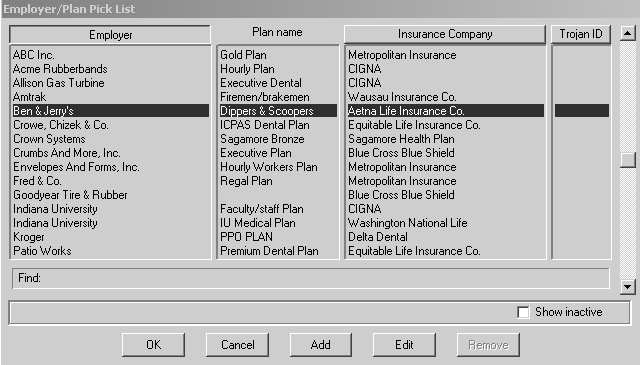
Select Lists > Employer/plans. The Employer/Plan Pick List window is displayed.
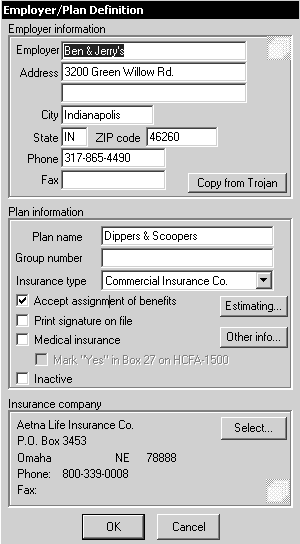
Select the Employer/plan and click OK. The Employer/Plan Definition window is displayed.
Click Estimating. The Benefit Table window for the employer is displayed.
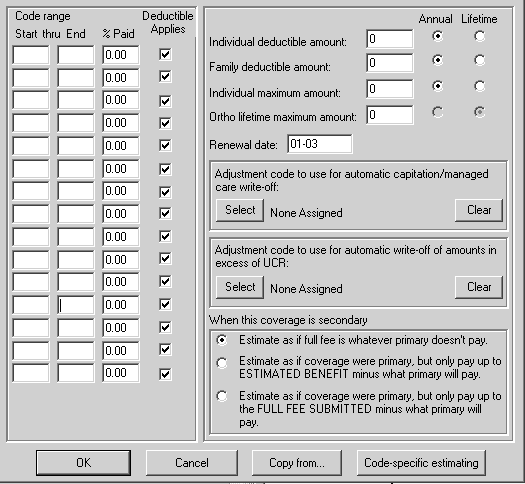
Click Code-specific estimating. The Benefit Details window for the employer is displayed.
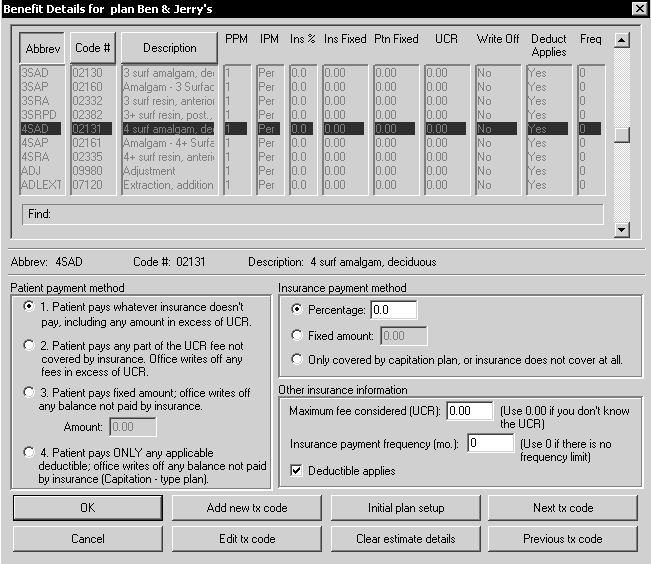
The Benefit Details window has the following four sections:
Code list
Patient payment method
Insurance payment method
Other insurance information
All data in the last three parts of the window apply to the code that is selected in the Code list.
Click Add new tx code to enter data for a new transaction code; click Edit tx code to modify data for the code selected in the Code list.
Select a payment method from the Patient Payment Method section:
Patient pays whatever the insurance doesn’t pay, including any amount in excess of UCR.
Patient pays any amount of the UCR fee not covered by insurance. Office writes off any fees in excess of UCR.
Patient pays a fixed amount; office writes off any balance not paid by insurance. If you select this method, enter the fixed amount in the Amount field.
Patient pays ONLY any applicable deductible; the office writes off any balance not paid by insurance.
Select a payment method from the Insurance payment method section:
Percentage
Fixed Amount
Only covered by capitation plan, or Insurance does not cover at all
In the Other insurance information section:
In the Maximum fee considered (UCR) field, type the UCR. If you do not know the UCR, type 0.
In the Insurance payment frequency field, enter the limit for how often the insurance company will pay for the code. The limit is defined in months. If there is no limit, type 0.
Select Deductible applies if there is a deductible.
Click OK.
Methods of Estimating Insurance
Benefit-Table Estimating by Plan